Colorectal Polyp / Polyps:
Why is it important to address this pathology?
Colon and rectal polyp is very common pathology seen during colonoscopy. The nature of the polyp / polyps (age of patient at which detected, size, location, number, family history, pathology and many more factors) decides the future course of action and the long term outcomes. Some of them can be cancerous too. Hence it is important to address this topic.
What is a colonic / rectal polyp?
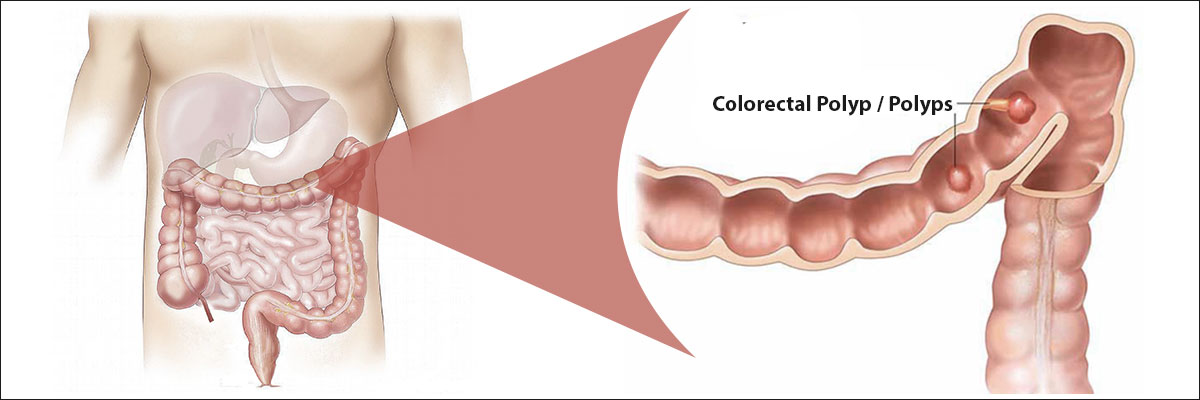
A polyp is a projection in the lumen from the inner lining / mucosa of colonic / rectal wall. (Polyp can occur in other places too i.e. gastrointestinal tract, respiratory tract, uterus, urinary bladder etcetera)
Why does a polyp form inside the large intestine?
There is no specific cause for polyp formation except for those associated with gene mutations & chronic inflammation. High fat diet, excess alcohol, smoking, obesity, infection are few associations. Majority of the polyps are sporadic / isolated in occurrence. Few are part of polyposis syndromes or following chronic inflammation as part of inflammatory bowel disease (IBD – Chrohn’s disease-CD or ulcerative colitis -UC). We are discussing here polyps which are tumors or have developed due to chronic inflammation (IBD).
Patients with certain inherited genetic changes (mutations) can have large number of polyps from young age sometimes from early childhood. This is known as polyposis syndrome. Family members (1st / 2nd / 3rd generation also some times) of these patients may also have this problem or are at high risk to develop polyposis. Patients with inherited polyposis syndrome have involvement of other organ systems too, depending on site of mutation on the genes involved. This includes brain tumors, thyroid cancer, gastric / duodenal polyps, liver tumors etcetera. Occasionally patients without known family history can also have these mutations (sporadic / de novo mutation) and may or may not pass it to the next generation.
In patients with IBD chronic inflammation at some point leads to uncontrolled cell growth and polyp or pseudopolyp formation.
What are the symptoms?
Patients may remain asymptomatic for a long time since it may take months to years for a polyp to reach a significant size or cause a problem. Most polyps are picked up as an incidental finding during a colonoscopy (endoscopy of large intestine) for various reasons like constipation, diarrhea, bleeding per rectum, abdominal pain or as part of health check up in asymptomatic patient especially after age of 50 years (incidental finding).
Large polyps may present with frank bleeding in stools, anemia due to chronic low grade blood loss in stools (occult blood in stools when stool is tested during investigations for anemia) or rarely constipation & abdominal pain. This is common to all age groups. Patients with polyposis syndromes can present with these complaints in their teens too. These patients are at a high risk to develop colorectal cancers at young age.
Is screening for colorectal polyps advised?
Screening for colorectal polyps is not advised as a routine process in the population. Patients above 50 years & otherwise average risk for colorectal cancer are encouraged to undergo a screening colonoscopy for polyps / cancer at least once in 10 years. Apart from this these patients are encouraged to do stool test for blood once a year. If that is positive then a colonoscopy is advised.
Patients with known family history of polyposis are advised screening colonoscopy from a younger age, once in 1-2 years and polyps are picked up early even before symptoms start.
Patients with known inflammatory bowel disease (ulcerative colitis / Chrohn’s disease) are advised screening colonoscopy around 8-10 years from the time of diagnosis. Depending on findings the frequency varies from once in 1-3 years.
When should you suspect a possibility of colonic polyposis syndrome?
If there are multiple polyps (>20) especially at younger age (before forty), one should rule out a polyposis syndrome. These patients may have more than 100 polyps and have a very high chance of developing cancer at young age. Such a patient is carefully worked up (family history, genetic analysis, features of other organ system – thyroid / brain etcetera) for polyposis syndrome. If established then family members (especially 1st generation) at risk are also counseled and encouraged to undergo work up to rule out polyposis / similar syndrome in them.
Are polyps benign or cancerous?
Colonic polyps can be benign / noncancerous, malignant / cancerous or there could be a small focus of cancer in an otherwise benign polyp. Some of the benign polyps are at high risk to develop malignancy (potentially malignant) than others. The risk factors include large size, peculiar endoscopic features, specific histopathological features of the polyp and associated genetic changes.
What is done when a colonic / rectal polyp is diagnosed?
The most important question is whether the polyp is benign or cancerous. Once found it is important for the patient to know the risk posed for cancer by the polyp, treatment needed if any and the surveillance / follow up needed if any. This is done on colonoscopy and biopsy. For better prediction of nature of polyp (& treatment) one needs a high end endoscopy system with in-built special technology (NBI, chromoendoscopy) , skilled & experienced gastroenterologist / endoscopist & experienced GI pathologist.
Most small nonmalignant appearing polyps (decided on endoscopic features) are initially snared and then sample is sent for histopathology or biopsy is taken by large forceps removing the entire polyp. Snares are better way of removing small polyps rather than random pulling with forceps. Larger polyps and malignant appearing polyps (decided on endoscopy) are usually biopsied in the 1st step and treatment is done after histopathology report. Treatment may be done endoscopically or through a surgery.
What special investigations are required in patients suspected with polyposis syndromes?
Patients with personal and family history / clinical suspicion of polyposis need special genetic studies to assess familial / hereditary problems. This is especially true for younger patients (<40 years of age). These include mutation in APC gene, MUTyH mutation and some uncommon gene mutations. The tumor tissue is also subjected to IHC for MMR status.
What is the treatment for benign non-syndromic / sporadic colorectal polyp?
Isolated small polyp/s (<10 in number) is/are usually only biopsied / snared. Benign appearing polyps more than 1 cm in in size are removed endoscopically in entirety and subjected for pathological examination. Once the benign nature is established then average risk patients are advised a surveillance program based on nature of polyps / risk of developing cancer (colonoscopy once in in 5 or 10 years). In experienced centers multiple polyps are also removed endoscopically.
Large or difficult benign polyps (after initial biopsy confirmation) need special endoscopic procedure (EMR / ESD ) for removal. These procedures need advanced equipment / set up, skills, experience, back-up support for difficult situations and complications; hence these should be performed only at specialized centers. After final histopathological confirmation of benign nature, again the surveillance instructions are given. If the final histopathology shows evidence of cancer then the polyp is considered a malignant / cancerous polyp and treatment is adjusted accordingly.
When do you need surgery for a benign polyp?
Some difficult polyps are unsuitable for endoscopic treatment and an upfront surgery is performed by open or laparoscopic or robotic way. Patient may develop a complication like perforation of intestine after endoscopic resection of a difficult polyp necessitating an emergency surgery. If an early malignancy is detected on final histopathology, then patient will need a surgery even after a successful endoscopic resection. Patients diagnosed with polyposis syndromes may need a complete removal of large intestine as they are prone for early malignancy. A surgery may also be required for a benign large polyp is it is removed only partially during endoscopy or is removed piecemeal and is found to have high risk features for cancer. Such a patient has an alternative of frequent follow up endoscopy.
What is the treatment of a malignant polyp?
A malignant polyp is a colorectal cancer & is treated on internationally accepted guidelines for colorectal cancer. This includes a pathology review of the biopsy, tumor markers in blood, molecular studies on biopsy specimen, imaging (MRI, EUS) investigations for staging before endoscopic removal (exceptional circumstances – very early cancer, medically unfit patient), local surgical removal or a major colorectal resection based on risk assessment / stage. Endoscopically / local surgically removed malignant polyps again are reviewed in detail with the pathologist and patient may be advised a formal surgery if needed on the risk assessment. For more information on colorectal cancer & surgery for colorectal cancer please read the section on colorectal cancer.
What is the treatment for polyposis syndrome?
Patients diagnosed at young age with huge number of polyps are at high risk of developing colorectal cancer at young age. Hence these patients are advised to undergo a prophylactic surgery even if they are asymptomatic (picked up in screening when known family history present). This surgery involves complete removal of colon and rectum at risk of developing polyps followed by joining of small intestine with anal canal. Few patients are at risk of requiring a temporary or permanent stoma (end ileostomy - bringing the end of small intestine to the surface). Few patients have their rectum relatively spared of polyps and opt for a surgery where rectum is preserved and entire colon is removed. Small intestine is then joined to rectum. These patients require diligent frequent screening of the remaining rectum. A second surgery to remove this remnant rectum may also be necessary.
Do polyposis syndrome patients need any other monitoring?
Polyposis syndrome patients need monitoring of stomach and duodenum for polyposis by doing upper GI endoscopy once in 2-3 years. Treatment depends upon findings and includes endoscopic removal or surgery. Apart from GI tract sometimes screening of other organs like brain, thyroid, liver, retina is also necessary depending on the genetic change found.
What are the possible complications in the endoscopic treatment of polyps?
Simple biopsy or snaring is usually not associated with complications except rare chance of bleeding which is usually controlled easily through endoscope. However special procedures like EMR / ESD done for larger polyps have more risk of bleeding and perforation of intestine.
What are the possible complications of surgery when required?
Please read answers to the questions on surgery for colorectal cancer
What is the surveillance / follow up protocol suggested for patients with polyps?
All patients with benign polyp/s are followed up at regular intervals (3-6 months / 6-12 months / yearly / 3 yearly / 5 yearly / 10 yearly) based on age / risk assessment, associated conditions like ulcerative colitis (UC) or familial syndromes like FAP.
Patients with familial polyposis syndromes, background of IBD need frequent surveillance endoscopy.

