Sequential Cardiac & Rectal Cancer Surgery
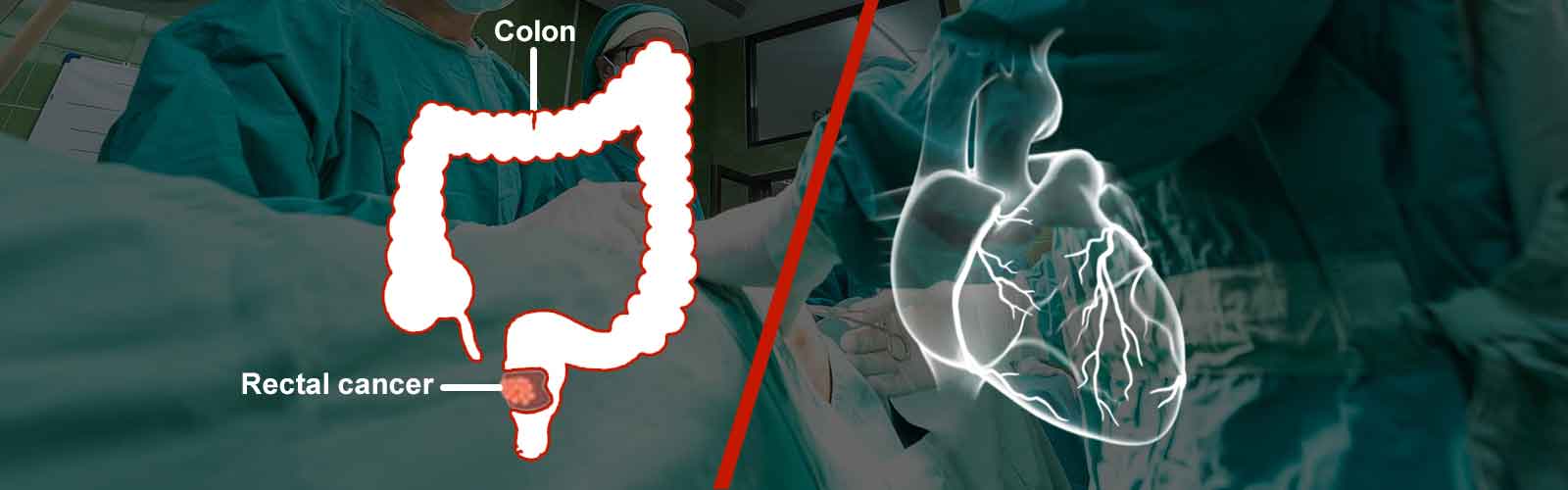
70 year old gentleman was diagnosed with ischemic heart / coronary artery disease & rectal cancer at the same time. The heart problem needed a bypass surgery and the rectal cancer a major abdominal surgery. The treating team of cardiologist and cardiac surgeon in consultation with our GI team drafted the treatment plan & family was counseled about it. A coronary artery bypass surgery was done as the 1st step achieving a successful cardiac revascularization. 7 days later patient was subjected to surgery for rectal cancer wherein rectum along with sigmoid colon was removed and intestinal continuity was reestablished by a coloanal anastomosis. The patient recovered successfully and was regularly followed by both GI and cardiology team for almost 6 years. Patient finally expired of reason unrelated to both cardiac / GI issue (brain stroke).
Rectal / left sided colon cancer is one of the commonest form of gastrointestinal cancers. Patients are usually elderly (>50 years). However young patients are seen too and these patients may have very aggressive tumors with poor prognosis.
Bleeding with stools is the commonest complaint. Some patients come with lower abdominal pain, bloating, gradually worsening constipation, weight loss, abdominal distension, weakness, complaints caused by drop in hemoglobin / anemia (tiredness / breathlessness / heart complaints – as was seen in our patient) etcetera. Acute intestinal obstruction is an emergency situation often seen with these patients. Sometimes patients present with advanced form of disease like spread to liver, lungs or ascites due to peritoneal deposits. The disease is seen to be more aggressive (mucin secreting, signet ring type and poorly differentiated) when it develops at a younger age and often is diagnosed at an advanced stage. Such disease has poorer prognosis / long term survival too. Patients with left colon / sigmoid colon cancer can also present like this.
Patients diagnosed or suspected to have a colon / rectal cancer are subjected to multiple tests. The most important ones are checking serum tumor marker CEA (carcinoembryonic antigen), colonoscopy and biopsy, CT scan of abdomen & pelvis and sometimes a PET CT study. The CEA is useful in diagnosing cancer and also to follow treatment response (surgery or chemotherapy). However all patients may not have a raised CEA. CT / PET-CT is done to see if tumor can be operated and removed or has it spread beyond the intestine in the surrounding area or distant organs like liver, lungs etcetera. A colonoscopy ( endoscopy of large intestine to visualize it from within) helps to take a biopsy and also checks whether cancer is in only one part or multiple parts of colon (synchronous primary tumor). The biopsy sample is run through many tests apart from regular histopathology. This includes immunohistochemistry (IHC) & genetic tests for mutations (KRAS, BRAF, microsatellite instability). These tests help in deciding prognosis, treatment plan, treatment sequence, chemotherapeutic drugs to be used. In short they have a major impact on treatment. However they are very expensive too.
Patients who have a localized disease undergo a curative colonic / colorectal resection (left hemicolectomy / sigmoid colectomy / anterior resection depending on which part is involved ). The surgery is performed as an open or laparoscopic surgery depending on the expertise available, extent of nodal disease and surrounding organ involvement / the bulkiness of tumor and patient presentation. Patients presenting with intestinal obstruction may need an emergency surgery, which may end in doing a colostomy (exteriorization of unobstructed part of colon as a temporary or permanent measure). Patients presenting with spread disease benefit with initial chemotherapy and it is later followed by a curative surgery where feasible. This is further followed by chemotherapy.
Multidisciplinary cancer care involves aggressive chemotherapy in the postoperative period (known as adjuvant treatment) or to downstage the disease (inoperable & / or unresectable disease to operable & resectable disease – neoadjuvant treatment) before any surgery. A chemoport (surgery) is inserted for delivering the chemotherapy to avoid problems of venous access. In neoadjuvant setting, chemotherapy is followed by a curative surgery where possible. Surgery is again followed by multiple cycles & lines (1st line, 2nd line etcetera) of chemotherapy. It is especially useful in young &/or fit patients with aggressive cancer disease. These patients can withstand the demanding nature of this treatment regime and may have better survival.
The patients are later followed on OPD basis initially every 3 months with CEA and USG report. A CT scan and colonoscopy is done once a year. The frequency of investigations and follow up is reduced after 2 years.

