Giant recurrent abdominal wall / ventral / incisional hernia
48 year old lady presented with recurrent abdominal wall / ventral hernia. She was 1st operated 15 years back for an umbilical hernia elsewhere when a mesh plasty was done through an open operation. She had recurrence in 2 years, however chose to continue with her problem for many years. She was operated for the 2nd time, when another surgeon performed a laparoscopic hernia repair and placed an intraperitoneal dual surface mesh. Unfortunately she developed hernia in the same place for the 3rd time. The hernia grew in size over 3 years before she presented to our team. A large portion of the small intestine was now outside the abdominal cavity (in the hernia sack). She had gained significant weight. She also had hypertension, hypothyroidism and diabetes. To compound the matters she had a short stature.
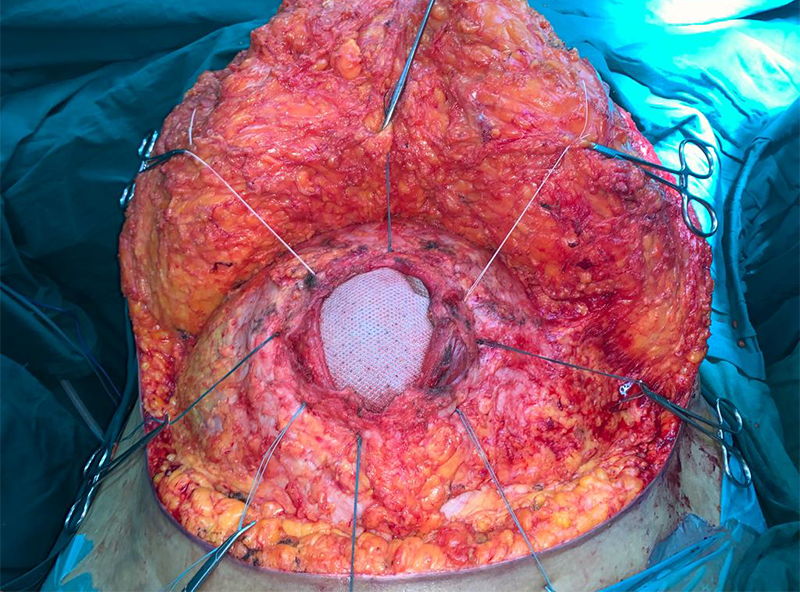
She needed another hernia repair, which as per our plan would be done in 1 or 2 stages. She would need a 2 stage surgery if an intestinal resection was felt necessary on the operation table so as to fit the intestines within available intra-abdominal space. She was counseled in detail about the surgery needed. She was also explained that she may need temporary ventilatory support after surgery due to increased intra-abdominal pressure. She was started on the mandatory respiratory exercise before the surgery for postop benefit. After thorough blood and imaging investigations she underwent the surgery. Both previously placed meshes were removed along with the hernia sac. Hernia defect was repaired using 2 meshes; one large dual surface mesh was placed intra-abdominally to bridge the gap in the abdominal wall and the another large mesh was placed extra-abdominally to reinforce the inner repair. The hugely pendulous abdominal fat pad was trimmed (abdominoplasty) giving the body necessary contour. She did not require an intestinal resection and ventilation due to the modified plan. She recovered well and was discharged on 8th day after surgery.
Hernia is a defect in the muscle through which underlying contents try to protrude out. When the defect is in abdominal wall muscles, then the hernia is called abdominal wall hernia / ventral hernia. The contents that try to come out of abdominal wall hernia are intestines and omentum. The defect can be congenital birth defect (e.g. umbilicus) or an acquired one. Factors that lead to an acquired defect are those that increase intraabdominal pressure repeatedly, over a long time, lead to weakness in abdominal musculature & over a period herniation of intraabdominal contents. Chronic cough, straining at passing urine e.g. due to prostate enlargement, chronic habitual constipation, lifting heavy weights for exercise, respiratory exercise that involve rapid movements of diaphragm / abdominal wall muscles (this includes certain exercises in YOGA), suddenly starting heavy exercise when not used to exercise are the factors that can lead to a tear / weakness in the abdominal wall & resultant herniation. These same factors can lead to a recurrence too after a surgical repair if proper precaution is not taken after the surgery. There is nothing against exercise or YOGA here. It is just that wrong method of exercise / wrong timing in life of starting certain exercise / exercise without supervision & without caution / overzealous exercise are the culprits in most situations
Abdominal wall hernia is a problem often taken very lightly without realizing that it can lead to complications like intestinal obstruction. Hence it is important to address it properly and in time too. If all the factors are not addressed properly at the 1st surgery then patient faces the risk of recurrence, which means another surgery. Every recurrence means more weaker tissues, more adhesions between hernia sac & intestine, more complex & difficult repair the next time, more risk of complications like bowel injury during surgery and more expense.
Abdominal wall hernia can occur in various parts, commonest being the groin / inguinal hernia and umbilical hernia (through the umbilicus or very close to it). Also common is incisional hernia (hernia through previous operation scar / incision).
The topic of discussion here is not standard inguinal or umbilical hernia but the recurrent hernia after a previous abdominal surgery or previous umbilical hernia repair. Most patients will have some discomfort bordering on pain, especially during exercise, coughing or walking. There will be a visible lump which is especially noticeable on coughing or increasing intra-abdominal pressure. Some patients present with intestinal obstruction due to intestines getting trapped inside a large hernia sac.
The only treatment for any hernia (including a recurrent hernia) is a surgical repair that will last. Abdominal hernia recurrence after a surgical repair as in above case is due to multiple factors. It is It is important to understand and address these factors when planning the next hernia repair / re-do surgery. These include the previous repair technique, mesh used / not, obesity, hernia size & contents, size of defect, status of abdominal wall muscles, patient factors responsible for recurrence (cough, constipation, obesity, lack of necessary precautions in exercise etcetera), pendulous abdominal wall etcetera. These factors decide the next technique, size and type of mesh, mesh position / location (intra-peritoneal / preperitoneal / over the muscles etcetera), use of special techniques like component separation / bowel resection / abdominoplasty for body contour etcetera, postoperative management (need for artificial ventilation, longer starvation, time of mobilization, use of abdominal wall supports and many more aspects)
Patient is thoroughly investigated from anesthesia, surgery and post-operative care point of view. Most important investigations are for cardiac function (echocardiography & stress test), lung function (spirometry – especially when patient has ongoing asthma / COPD), renal function, liver function, thyroid function, diabetes control & surgical planning (CT scan of abdomen & pelvis). Once completely investigated, the patient and family are counseled about the treatment / surgical plan (number, size, type & position of mesh, need for component separation if any, need for intestinal resection & adhesiolysis if any, need for abdominoplasty if any, possibility of removal / refashioning / relocation of umbilicus, possibility of temporary artificial ventilation in the postoperative period, risk of surgical complications like bowel injury / infection / bleeding, need for a 2 stage surgery if any).
This is an open surgery done under epidural and general anesthesia. The surgery is planned in such a way that most often the scar is cosmetically located in the bikini line over the lower abdomen. The defect is identified & hernia contents are returned to abdominal cavity. Bowel resection is avoided as much as possible and is reserved for carefully selected patients. These patients have most of their intestines in the hernial sac meaning practically outside the abdomen. Suddenly pushing them back and closing the tummy under pressure can cause low blood pressure requiring supports & inability to breathe comfortably meaning need of artificial ventilation. In such patients occasionally part of small or large intestine and omentum (fat curtain) will be removed. Defect is closed with local tissues, separating muscles of abdominal wall (component separation) or using a double surface mesh (one that has an inner surface compatible for intestinal contact and an outer surface for muscle contact). The umbilicus is relocated, refashioned or removed. Excess skin with fat is trimmed for cosmetic reason. Few drains are placed under the skin flaps to remove devitalized / dead / liquified fat. They are removed in due course after the surgery. Pain in the postoperative period is controlled with epidural analgesia (catheter in the back), intravenous painkillers or oral analgesics. Patients typically will be in the hospital for 7-10 days. Patients who need intestinal resection will undergo 2 stage surgery and the final repair is done in the 2nd stage. In these patients and those who require postoperative ventilation will stay longer in the hospital.
The advantage of all these precautions usually results in a rapid recovery, a lasting repair & a cosmetic scar.
After the surgery the patient is advised to use an abdominal support during all the activities, if possible a customized corset; avoid straining of all sorts (constipation, lifting heavy weights / travel bags / child, certain exercises etcetera). However patient is allowed most of the routine activities and is back to normal life.